
If you were wandering the 6th-floor of Scaife Hall searching for Pitt’s famous pathology chair in the 1960s, you wouldn’t have had to look for long. Emmanuel (Manny) Farber—whose reputation preceded him due to his breakthrough studies of chemical carcinogenesis and his instrumental role in taking on the cigarette industry—had the kind of penetrating voice that carried down the corridor. That was especially the case when he was excited—and on the job, he always was.
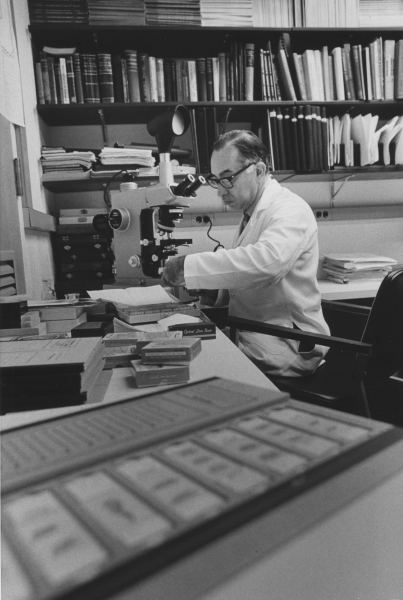
Every morning at 10:30, Farber—a dynamo, about 5’ 7”, who lived his life on fast-forward—would gather the pathology pack around a fresh pot of coffee and a carousel of slides. Mostly liver-cancer researchers like him, the scientists assembled for a uniquely open confab, with faculty, grad students, and postdocs alike encouraged to speak up, and often.
But, if you didn’t lead with verifiable data—peer-reviewed, published, and replicated to Farber’s satisfaction? That, he insisted, was not science, but “BULL ... !”—and he’d let you know, in so many words.
Well, exactly one.
There were, in a sense, two Farbers: One, a departmental uncle, a mensch who was not above wearing a Santa suit (though he was culturally Jewish) at the parties he hosted in his Pittsburgh home, where his wife, Ruth, played the piano. A scientific shepherd who over the course of his career served as president of the American Association for Cancer Research (AACR); editorial board contributor at numerous cancer, liver, pathology, and biochemistry journals; and a member of too many panels and societies to mention. A man who, in the days before strict rules about grant reviewers and applicants steering clear of each other, would simply call an investigator up and say, Hey, I think there’s a better way to go about this, and step in to try to help.
And then there was the other Farber, the no-nonsense academic who so abhorred superficiality, and so delighted in the sport of scientific sparring, that he rattled his colleagues’ and mentees’ nerves, often with a devil’s advocate shtick that was all too convincing. He might use his favorite one-word retort on you, for example, when discovering that you had an animal model of a disease. He’d scoff, question how a rodent could be useful in the study of complex human pathogenesis. How does that relate?! In the meantime, he himself was working on a new rat model of liver cancer.
Farber came to Pitt from Tulane University in 1961 to fill the sizable shoes of Frank Dixon, the Jonas Salk recruit who had built in Pittsburgh one of the premier research-focused pathology programs in the country. (Dixon had left for an appointment as founding chair of experimental pathology for the Scripps Clinic and Research Foundation in La Jolla, Calif.; he then led what would become the Scripps Research Institute.) Pitt pathology at the time, like Dixon, had a big immunology bent—so big, there was room for little else. Farber changed all that, building a full-fledged academic department ingrained in what he called biochemical pathology, the close study of the chemistry, anatomy, and physiology of cells in the presence of disease.
By the time of his death in August 2014 at age 95, Farber had garnered such honors as the inaugural fellowship of the AACR Academy, bestowed just shy of the 50th anniversary of the 1964 surgeon general’s report on smoking and health. He served on the committee that authored the report, which remains one of the most important publications in the history of public health.
***
Farber, who completed med school and trained in pathology in his native Ontario, Canada, realized early on that his specialty presented a unique window into the mechanisms of disease processes, an exciting, problem-driven mode of medicine. At UC Berkeley he completed a PhD in biochemistry, a move that was almost unheard of for pathologists at the time.
Farber did early work on the biochemistry of cell death and was among the first to observe it as an active process involving the cell’s own biochemical/metabolic processes. He also showed that carcinogens can bind to nucleic acids, which then create specific DNA adducts. He demonstrated chemical carcinogenesis as a chain reaction, establishing a disease model that followed a predictable series of sequential steps.
The progression of these steps would later prove to have predictive value, in terms of understanding how aggressive a cancer would be, says Richard Hegele, chair of pathology at the University of Toronto, where Farber was chair emeritus and professor when he died. Such insights proved helpful in determining which therapy would work best for a given case—contributions that “evolved toward precision medicine,” Hegele says.
Ezio Laconi, professor of pathology at Italy’s University of Cagliari, who was a PhD student in Toronto when he first met Farber, says his former chair’s greatest legacy is a fundamental principle of cancer biology that in recent years has been gaining new appreciation. And that principle is: Context matters.
Before a tumor appears, usually there are alterations in tissues, says Laconi, because they’ve been “suffering for a long time” from stressors like inflammation—conditions that create “optimum soil” for the emergence of cells that progress toward cancer.
In his Pittsburgh lab, Farber launched investigations that would lead to his greatest claim to fame, the Solt-Farber resistant hepatocyte model of carcinogenesis. It begins with the liver, a unique organ that, when healthy, can regenerate to its original size, even if you remove as much as two-thirds of the organ. Farber and his collaborators found that if you do so chemically and using certain toxic agents that are known to halt cellular proliferation, the liver regenerates anyway—but bulks back up with cancer cells instead.
“That was a famous discovery for liver biology,” says Pitt’s current chair of pathology, George Michalopoulos, an MD/PhD and Maud L. Menten Professor of Experimental Pathology.
“This [liver model] has been studied all over the world,” notes Henry Pitot, former director of the McArdle Laboratory for Cancer Research at the University of Wisconsin, Madison, adding that researchers like to use this particular model because it yields precancerous areas within weeks instead of months or years.
For Laconi, this finding, which was published in Nature in 1976, had far grander significance, presenting a new paradigm: When a toxin poisons the body continuously over time, robbing a given tissue’s cells of their ability to multiply, what’s left standing is a very small number of stubborn, embattled survivors—the cockroaches of cell life. Farber believed that, in the great majority of cases, precancerous cells are a response—an adaptation—to toxicity. For adults older than 50, most cancers are “certainly explainable, at least in principle” with this concept, says Laconi, pointing out that most known risk-factor agents are toxic in nature: UV exposure, certain viruses, and of course smoking.
“As Dr. Farber used to say, one of the main features of biological systems is, they react,” says Laconi. “They try to adapt to environmental conditions.”
***

"I never thought I would be a pathologist,” says Stewart Sell (MD ’60), professor of biomedical sciences at University at Albany, SUNY. “Who wants to sit around and look at a microscope all day? But [at Pitt] it wasn’t just looking at slides or making a diagnosis. It was thinking about how these things happened. And, how could you set up an experiment that could show how these diseases occurred? That stimulus was fantastic.” Sell returned to Pitt as a junior faculty member. At the time, the immunologist wasn’t particularly interested in hepatocarcinogenesis, but the lively discussions reeled him in. “I started a project in liver cancer that led to a continuing interest. We are still funded for this.”
In 1965 Farber secured $30,000 from the National Institutes of Health to make Pitt the host of a first-ever conference on “biochemical pathology,” held at Seven Springs resort. Forty scientists from seven countries came in June to present papers, which were published in a seminal book the following year. “One of the potentials of the field,” the press release read, “is the detection of disease-caused changes in cells before the disease becomes clinically evident in the patient.”
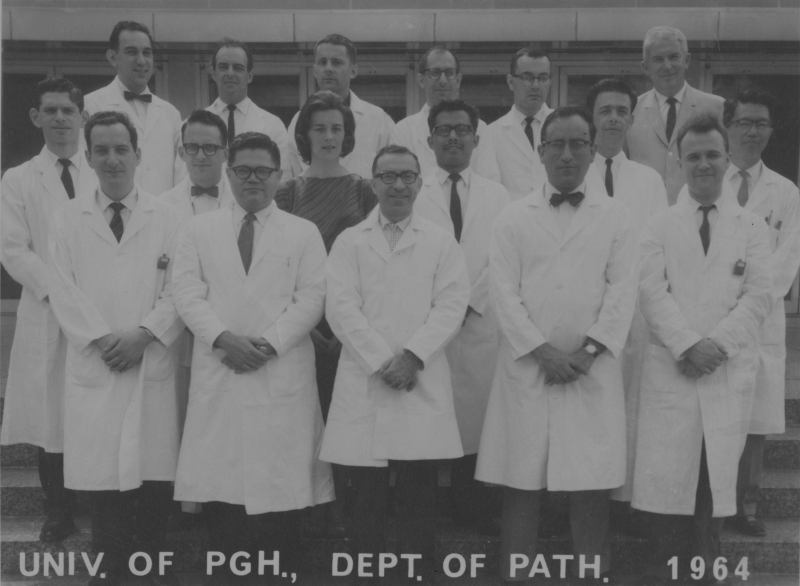
With Farber at the helm, Pitt’s crew of academic pathologists had an uncommon abundance of time to devote to their studies, while maintaining close ties to the clinical pathologists. Many in the department at the time would rise to prominence in the field: Nobuyuki Ito (Fel ’64) became dean of Nagoya City University Medical School in Japan; Bob Kisilevsky (PhD ’69) is professor emeritus of pathology and molecular medicine at Queen’s University in Ontario; Mike Lieberman (MD ’67, Res ’70, PhD ’72) was pathology chair at Baylor and founding director of the Houston Methodist Research Institute; Benito Lombardi and Hisashi Shinozuka founded the carcinogenesis research section of Pitt’s Division of Experimental Pathology; Frank Sherman (MD ’38) directed pathology at Children’s Hospital of Pittsburgh of UPMC; Herschel Sidransky chaired pathology at George Washington University; and Robert E. Lee (MD ’56) served as pathology professor at Pitt.
In high school and college, Joe Locker (A&S ’67) worked next door to Farber in the lab of Joseph Leighton (who would, by the way, go on to chair pathology at Medical College of Pennsylvania, which was later absorbed by Drexel University). Locker is now a pathology professor at Pitt. “Manny took an active interest in my scientific development," Locker says, “and we had a lot of scientific contact over the next 40 years.”
Throughout Farber’s career, he reached out to chemists, physicists, microbiologists, mathematicians, and others. Multidisciplinary brain trusts are commonplace in pathology departments today, but at the time, people thought the idea was “crazy,” recalls Sarma Dittakavi, who first met Farber as a postdoc at Pitt in 1965, and was then recruited by him, twice—first when Farber left Pitt to direct Fels Institute for Cancer Research & Molecular Biology at Philadelphia’s Temple University in 1970, then when Farber returned to his alma mater, University of Toronto, as pathology chair in 1975.
As a trainee, Mike Lieberman fell for Farber’s enthusiasm hook, line, and sinker. Presbyterian Hospital’s pathology chief had told the up-and-comer that what he really needed to satisfy his natural curiosity was a research project—so he should go talk to Farber. Within 30 minutes, Farber convinced him to do a new combined residency/PhD program he had started, one of the first of its kind in the country. “I never regretted it,” Lieberman says.
Fun Farber fact: Previously, he had also founded a PhD program at Tulane, its inaugural enrollee being Pitot, who went on to mentor Pitt’s own Michalopoulos. “He gave me great leeway,” recalls Pitot—so he paid the favor forward. “I gave [Michalopoulos] the bit, and said, ‘Go,’ and he’s become an expert in the field.”
Michalopoulos met Farber as a resident in Wisconsin. Farber “was always very helpful,” he says of his scientific grandfather. Once, Michalopoulos wrote a grant that included a salary for a technician—which Farber advised him to nix. “And he was right. We were forced to dig in and get the results [ourselves]. If they were coming to us served on a platter, we probably would have missed them.”
***
On the front page of the April 26, 1961 Pitt News, the student newspaper ran a story about the appointment of Emmanuel Farber as pathology chair. On the back of that same issue was a half-page ad for Tareyton cigarettes, bragging that their dual filter was “definitely” proven “to make the taste of a cigarette mild and smooth.”
This was the tobacco industry’s new MO: outwardly denying the fact that their product was anything less than healthy; internally circulating memos about the urgent need to develop “a medically acceptable cigarette,” pronto; and promoting the hell out of their new filtered cigarettes, which they hoped would sidestep the problem altogether—of course, to no avail.
In Philip Morris’s pocket were experts from premier universities who would attack any smoking-related science of substance. Cigarette producers sent pro-tobacco broadsides to 200,000 clinicians and ran ads featuring lab-coated docs lighting up. In the middle was the public, confused and swept up in misinformation.
The stakes could not have been higher. It was time to call “BULL!” on Big Tobacco.
On November 9, 1962, Surgeon General Luther Terry and his deputies convened for the first time with 10 scholars (selected from an original list of 200 names put forward by private health and government officials). The committee’s charge: to vet the entirety of the relevant scientific literature to date—some 7,000 articles. Among the 10, Farber was the “most original thinker,” writes Richard Kluger, author of the 1996 book Ashes to Ashes. (He also quotes the committee’s scientific coordinator, Peter Van Vechten Hamill, who called Farber “a volatile little guy with a highly superior IQ.”)
In the modern-styled National Library of Medicine in Bethesda, Md., the committee convened nine sessions of two to four days each over the course of 13 months. They usually got together in the mezzanine, or in the third subbasement, where as many as 30 staffers at a time (each with government clearance) typed and copied and clamored around the clock. Armed guards secured the building.
In analyzing 36 population studies, the committee and their armies of consultants found that smokers died of lung cancer at a rate 10.8 times higher than nonsmokers. And that the more people smoked—and, the longer they kept at it—the greater the risk of lung cancer. And that this was the case no matter who you were, where you were from, what your socioeconomic standing was, or what the air quality was like in your town.
Before committing what became their famous tome to paper, the committee had one lingering issue to settle: the American Cancer Society–funded study, which was integral to their case because it combined epidemiological and histological evidence (including samples from both humans and experimental animals) so beautifully ... perhaps too beautifully. The study was troublingly perfect.
Farber wanted to see the specimens for himself. So off to New Jersey he went.
For two days, Farber led the effort to scrutinize the slides—the last day running from 4:30 a.m. to 10 p.m.—until he was satisfied. Though there weren’t fully formed tumors (the animals often died first from the poison of the smoke), the start of cancer was there, in the form of cellular changes he was familiar with. (Throughout his career, he was always a strong proponent of the importance of dynamic, whole-organism studies.) And, to everyone’s relief, the samples, in Farber’s fastidious assessment, were carefully and honestly come by.
Months later, the U.S. government published the report in a secure, fenced facility, and Terry released the document to the public. To date it has still done more to prevent smoking-related disease than any other preventive measure.
But if you ask Farber’s friends and family, he never bragged about it. “He thought it immodest to talk about himself,” says his daughter, Naomi Farber.
***
You’d hear it in the hall, recalls Lori Cutler of the 11 years she spent at the IBM Selectric typewriter outside Farber’s office at the University of Toronto. ONCOGENES?! WHAT ONCOGENES?!
“He’d be yelling,” she says. “I’d be on the phone, and [the person on the line] would say, ‘Who’s that?’ And I would say, ‘Oh, that’s my boss.’” Cutler pauses, cutting up. “The secretary beside me would say, ‘Here comes Dr. Farber with his BULL … !’”
Farber enjoyed arguing for the sake of arguing, it’s true. But he was also known to fundamentally disagree with colleagues.
He disagreed with Pitot about how cancer arose in the liver.
He disagreed with Lombardi about the significance of what are called oval cells, which Sell eventually showed to be liver cancer stem cells. Ironically, Farber, who’d actually discovered the existence of oval cells and gave them their name, was sure they were ductal cells and nothing more. “It was kind of sad for me,” says Sell. “He could have had much more credit, if you will, for this whole idea.”
And, from the 1970s on, Farber disagreed with seemingly everyone when it came to oncogenes—the genes that can act like accelerator pedals for cancer. “BULL!” etc. “What’s the evolutionary advantage of that?!”
As the initial theories about the genetic origins of cancer were cropping up, Farber was unconvinced. He said: You can’t explain tumor formation with a single event. “And in my opinion, that was correct,” says Laconi. “Those simplified approaches are not getting us very far . . . particularly, in our ability to cure cancer. There are a few examples where genetic approaches have given some results, but overall we’re nowhere close to what we were hoping for when Richard Nixon declared war on cancer in 1971.”
As cancer research waded deeper into oncogenes, Farber couldn’t abide it. But he continued to grow and thrive nonetheless.
“My dad had this philosophy,” says Naomi Farber. “Do something, give it your best, transform it, and then move on.”
After a decade as pathology chair in Toronto, in which he grew the graduate program from a handful of people to more than 150 students, he stepped down to focus on his research and his teaching. In his leadership roles in his department, as well as the broader pathology community, he fostered the development of subspecialties in the field: experimental pathology, biochemical pathology, and toxicologic pathology.
And he brought undergraduates into the fascinating (albeit often grim) world of pathology. He designed a “Principles of Pathobiology” course, a problem-oriented way of teaching life sciences—and it was a runaway hit, growing quickly from 40 to 140 students per semester. The class started in 1978 and is still going strong in Toronto.
In examining slides and sometimes even whole organs, the students found context for the content they were learning and came to appreciate the features of normal versus diseased specimens side by side: controls versus the lungs of a miner or the liver of an alcoholic. And invariably, several students quit smoking by term’s end, notes Dittakavi, who cotaught the class with Farber for many years.
Cutler came into the lecture hall to help set up for the class a few times and stayed to be awed by the boss who was like a father to her. When he got stirred up, the tempo, pitch, and volume of his voice would uptick. “His eyes would light up when he would see all these students in the room eager to take the course.”
“His enthusiasm was contagious, especially for young people,” says Laconi. “He was, in Italian we say, a faro, a lighthouse. He illuminated my path to research.”
Cigarette advertisements from the Collection of Stanford Research Into the Impact of Tobacco Advertising. Photos Courtesy Naomi Farber.
Burning Issue
BY ELAINE VITONE
In 2014, Acting United States Surgeon General Boris D. Lushniak released The Health Consequences of Smoking—50 Years of Progress. Data on smoking’s effects are detailed in the new document, the contributing authors of which include Nancy Davidson, University of Pittsburgh Cancer Institute director, president of the American Association for Cancer Research, and Pitt’s Hillman Professor of Oncology; Steven Shapiro, chief medical and scientific officer for UPMC and Distinguished Professor of Medicine at Pitt; and Hilary Tindle, former Pitt assistant professor of medicine, epidemiology, and clinical and translational science (now at Vanderbilt). A few highlights:
- Smoking is still the biggest cause of preventable death and disease in the United States.
- Smoking rates among adults and teens are half of what they were in 1964, and today’s smokers don’t smoke as many cigarettes. However, because of changes in the composition of cigarettes, smokers are at an even higher risk for lung cancer now than 50 years ago.
- Adding filters to cigarettes has done more harm than good. Because they cut irritation, filters encourage deeper inhalation. And some of the 69 known carcinogens in this toxic smoke are at even higher levels in today’s cigarettes.
- Women are now in just as much danger of dying from smoking-related diseases as men, for the first time in history.
- In the last 50 years, more than 100,000 infants have died of SIDS, conditions associated with premature birth and low birth weight, and other obstetric complications resulting from parental smoking.
- The economic cost of smoking is approaching $300 billion annually—and climbing.
- We now know that smoking is linked to diseases in almost every organ in the body.
Nico-Ween
BY ELAINE VITONE
Nicotine withdrawal isn’t pretty: irritability, tanking mood. And the so-called “light” cigarettes on the market give smokers no leg up in cutting down. Studies show that these products, which differ from their counterparts only in their ventilation systems, just train smokers to inhale more deeply and more often.
But a six-week study published in the New England Journal of Medicine in October showed that if you instead reduce the amount of nicotine in cigarettes, smokers don’t experience the usual fallout. Those who were given smokes with less than 15 percent of the usual dose actually lit up 23 to 33 percent less, and with “minimal” signs of withdrawal. A month later, these smokers were twice as likely to have tried to quit again, compared to controls who smoked cigarettes with typical amounts of nicotine.
The preliminary study made a splash in the national media, and since then, several long-term follow-up trials have continued to build the case for FDA regulations on nicotine levels. If enacted, such legislation could have an “enormous” impact on public health, says lead author Eric Donny, a PhD professor of psychology with a secondary appointment in psychiatry at Pitt. “One model predicted that the prevalence of smoking in the U.S. would fall to under 5 percent.”
Smoke and Mirrors
BY KRISTIN BUNDY
In 2005, the University of Pittsburgh’s Brian Primack had just wrapped up a public health class on cigarette smoking; and a student came up to him, saying, “I don’t know if you know this, but hookah [or water pipe smoking] is what we all do now.” At that time, Primack says, hookah use was flying under the radar, and e-cigarettes had not yet entered the market in the United States.
Motivated by that after-class discussion, Primack, MD/PhD professor of medicine, pediatrics, and clinical and translational science, began to study the prevalence of hookah smoking—and later e-cigarette use—among middle school, high school, and college students. What he found is that young people believe vaping and hookahs are more socially acceptable than smoking cigarettes. They also see them as less harmful and less addictive—Primack has found otherwise. (Note the Royal College of Physicians is now recommending that cigarette smokers switch to vaping; that stance is not shared by FDA officials who will begin regulating all tobacco products this August.)
Data published by Primack in Public Health Reports and JAMA Pediatrics showed that water pipes are more toxic than cigarettes, and vaping is a potential new gateway to smoking, even for young people who said they never intended to smoke traditional cigarettes.
One allure for the young set is that vaping, as well as hookah tobacco, can have a fruity or candylike flavor. And overall there are few negative social implications or media influences.
Primack is working to change that. In his roles as Pitt’s assistant vice chancellor for research on health and society and director of the Center for Research on Media, Technology, and Health, he’s reaching out to empower youth—teaching them to analyze how the tobacco industry can manipulate people through advertising, educating them on the risks of these devices, and hopefully extinguishing the temptation to experiment altogether.
In the meantime, he notes, as more adults heed smoking warnings and put their butts out for good, more young people could be getting hooked.
