 Okay, this sounds weird: A researcher at Pitt has managed to grow working livers—and other organs—in animal lymph nodes.
Okay, this sounds weird: A researcher at Pitt has managed to grow working livers—and other organs—in animal lymph nodes.
The scientist’s name is Eric Lagasse; he’s a PhD, a PharmD, a professor of pathology at the School of Medicine, and the director of the Cancer Stem Cell Center at the Pitt-UPMC McGowan Institute for Regenerative Medicine. He’s been doing fascinating studies with partners Paulo Fontes, MD associate professor of surgery who directs the machine perfusion program at the Thomas E. Starzl Transplantation Institute, Massimo Trucco, Hillman Professor of Pediatric Immunology, and, among others, Junji Komori, an MD/PhD postdoctoral fellow in the Lagasse lab who was one of the lead authors on a recent Nature Biotechnology paper on these breakthroughs.
First, what's at stake: Each year in this country, doctors diagnose 65,000 people with end-stage liver disease; many of these people have cirrhosis. The only cure is a liver transplant, yet only 6,500 liver transplants are performed each year.
Beyond the liver, preliminary success with cells from other organs, including the pancreas and thymus, could also have dramatic implications for human health. Think help for patients with diabetes or who are immunocompromised. Lagasse’s approach might even work as a way to wean transplant patients from immunosuppressive regimens.
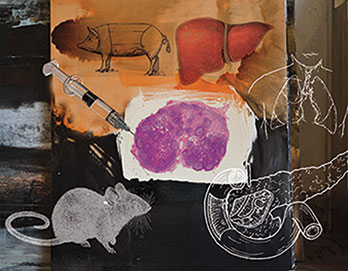
What made Lagasse think of this? In an experimental attempt to treat liver failure in a mouse, Lagasse’s team was injecting healthy hepatocytes (liver cells) into its spleen. Sometimes, the researchers inadvertently missed the spleen, and the cells were injected into the belly. They learned those cells had migrated to the lymphatic system, where they formed colonies.
So, naturally, he thought: “Maybe if we could generate a functioning liver outside of the liver, that would be an option for patients.” In fact, other researchers have been attempting to grow liver tissue (and that of other organs) elsewhere in animals using transplanted cells for some time with limited success. Some of the difficulties have involved obtaining enough donor cells, keeping the transplanted cells viable, and—in the case of liver studies—generating enough liver mass.
What they did: Injected 100,000 to 500,000 hepatocytes into the lymph node of a mouse. Animals don’t seem to get cirrhosis, and there’s no animal model of the disease, so Lagasse’s team used a mouse model with genetically induced liver disease. That one injection generated enough mass to rescue the animal from the disease.
The mouse grew a new, functioning liver, right there in the lymph node. Lagasse’s team repeated this dozens of times. Their model in larger animals is also promising.
How does a body make enough space for a new organ? Especially something as massive as a liver? There are plenty of lymph nodes in the abdominal cavity, and there’s also plenty of space for an extra liver, Lagasse assures. Also, hepatocytes don’t grow out of control like cancer cells do; they only grow as needed. They innately seem to seek out equilibrium. For example, if a mouse has a liver that’s functioning at about 40 percent, the new lymph-node-hosted liver will tend to be 60 percent of normal size. And when Lagasse’s team removes more of the native liver, the surrogate livers in the lymph nodes grow again to make up for that loss of tissue.
As good as this sounds, Lagasse doesn’t see this as a way to replace a liver. These surrogate livers have vasculature, but there’s no biliary system—no bile ducts or other way to get rid of bile juice. (Which makes sense: What would the biliary system connect to?)
How he imagines these surrogate livers working, someday. As an auxiliary liver that helps the native diseased liver repair itself.
Could a surrogate organ lead to a blocked node, like what happens in lymphedema? Lagasse says, “We have not seen any lymphedema in our animal models. We believe that the ectopic organogenesis [surrogate organ growth] prevented this problem by rerouting the lymphatic drainage.”
What are the chances—assuming the lymphnode-hosted organ approach proved safe in humans—that a patient might end up with a second diseased liver? “To be frank, we do not know,” says Lagasse.
“Our hypothesis is the liver tries to regenerate, but the environment is so destroyed, there’s no way that it can do so. The idea here is by transplanting cells into a lymph node, which is basically a virgin environment, we will be able to generate a functional liver.”
But they won’t know until they actually try it in patients.
If the lymph node is used as a bioreactor, can it still do its day job, i.e. fight off disease? The human lymphatic system has 500 to 600 lymph nodes, so using one or two for organ growth shouldn’t hinder its abilities, note commentators from Nature Biotechnology. Lagasse’s team has shown the novel approach doesn’t seem to impede immunity.
What about rejection? The lymphatic system is a strategic stronghold in the fight against disease, where T cells and B cells garrison to launch attacks against invaders. Wouldn’t placing newly transplanted cells there be asking for trouble? Apparently not. The procedure works fine in animals when given an immunosuppressive regimen.
What’s good for the liver is good for the pancreas and thymus. . . A preliminary study with Massimo Trucco involved a monkey with diabetes. The animal had normal blood glucose levels after the research team transplanted islets (a type of pancreatic cell) into a lymph node. After three months, researchers detected the presence of islets in the lymph node along with insulin-producing beta cells.
If your thymus, generator of T cells, doesn’t work, you become immunocompromised. When Lagasse’s team transplanted thymic tissue into lymph nodes of mice born without a thymus, the mice were able to generate functional T cells that rejected tumor cells or skin grafts from other mice. (PhD postdoctoral fellows Aaron DeWard and Lindsey Boone contributed to these studies.)
An eye toward ending the rejection issue altogether. Lagasse thinks he’s found a way to trick the immune system.
In addition to transplanting thymic tissue into a lymph node to treat immunocompromised people, he’s experimenting with this surrogate organ technique as a way to “reeducate” the immune system so it won’t reject transplanted organs.
Here’s the idea: Imagine you need a new liver. You are approved for a transplant. Your surgeons give you immunosuppressive drugs. They take a piece of the thymus from the liver donor and transplant it into your lymph node. At the same time, they do the liver transplant. The thymic tissue starts to function in its new habitat, and after a while, your body learns to accept the donor liver without the immunosuppressive regimen. Lagasse has not published on this yet but says that the system is working in mice.
Biggest obstacle to moving forward: It’s not a question of immunology, or physiology, or anything scientific, says Lagasse, who is eager to translate his findings to the clinic. His biggest roadblock of late—diminishing funding.
What keeps these researchers inspired: The huge need—there are tens of thousands on waiting lists for new livers. And Fontes, the surgeon, adds that more than 30 percent of patients with end-stage liver disease can’t even get on the transplant waiting list—they have no alternative. “This technology could be a new therapeutic option for this severely underserved patient population,” he says.
“A liver transplant is an incredible operation,” says Lagasse. “But most people with end-stage liver disease won’t get a transplant. They will die.
“The people who are really excited about this are the surgeons who see patients, see the outcome of liver disease, and really understand what we are trying to do.”
Breathe Easier
Artificial Lungs Are Helping Patients
By Natalie Ernecoff
 William Federspiel scoops sugar into his coffee and sits down for an interview regarding the Hemolung, an artificial lung his team has designed.
William Federspiel scoops sugar into his coffee and sits down for an interview regarding the Hemolung, an artificial lung his team has designed.
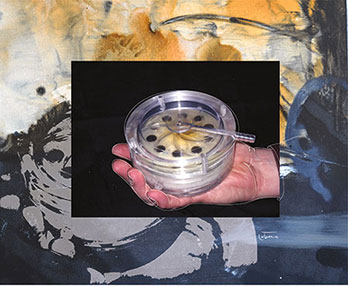
As he reaches for a coffee stirrer, he says, “You put sugar in your coffee. If you want it to dissolve faster, you stir it more vigorously. What’s unique about the Hemolung is that in the design we employ active mixing. A rotating cylindrical core disturbs the blood flow patterns. By adding that additional movement, you can increase the rate at which CO2 moves from the bloodstream and oxygen moves into the bloodstream.”
Federspiel, a PhD, Whiteford Professor of Bioengineering with secondary appointments as professor in critical care medicine and chemical engineering, says that the Hemolung requires only a small amount of blood flow outside of the body, in contrast to previously available methods that are substantially riskier.
Since gaining approval in Europe, Australia, and Canada earlier this year, the device has helped approximately 30 patients.
The Hemolung works via a catheter that can be inserted by a physician in the intensive care unit. This access point allows blood to flow through a cartridge containing hollow, hair-like fibers. As blood runs continuously through the module, pure oxygen is pumped inside the fibers. Oxygen and carbon dioxide are exchanged using the hollow fibers, with augmentation from the rotating cylinder (recall the coffee stirring example). Federspiel notes, “That’s what enables it to remove what seem to be clinically significant levels of CO2 at relatively low blood flow rates.”
Years ago, Federspiel helped found the Pittsburgh-based ALung Technologies with the late Pitt surgeon Brack Hattler. ALung developed and manufactures Hemolung. (Federspiel is an equity holder in the company.)
Federspiel and colleagues recently received a $3.4 million National Institutes of Health grant to develop a wearable artificial lung. Similar in function to the Hemolung, this module (Paracorporeal Ambulatory Assist Lung, or PAAL) would be contained in a single unit that could be strapped over a patient’s shoulder or around the waist.
“It would be an integrated, compact artificial lung that could be worn by the patient. That’s the goal,” says Federspiel.
Unlike existing respiratory support devices, the wearable lung would allow patients to move about relatively freely in the hospital and perhaps, eventually, in their own homes.
Though not intended to be permanent, the wearable PAAL could act as a bridge for patients waiting for a transplant. And it could help both acutely and chronically ill people increase their chances of receiving a transplant by maintaining their health in the interim.
The Latest Heartthrob
Grown in a Lab
By Jenifer Lienau Thompson
 Be not still, spontaneously beating heart!
Be not still, spontaneously beating heart!
For the first time, researchers have used stem cells to build heart tissue that started to beat on its own, with nary a jump start. What’s more, the stem cells figured out on their own what types of heart cells they needed to become.
For three years Lei Yang, assistant professor in Pitt’s Department of Developmental Biology and director of the Stem Cell Core, has labored with his colleagues Tung-Ying Lu and Bo Lin to design a new process for engineering human heart tissue. But these PhD researchers are not satisfied with mere tissue— they aspire to grow whole hearts, personalized for implant in patients suffering from end- stage heart disease.
“Heart disease is the leading cause of death worldwide,” says Yang. “Transplant therapy is limited by the availability of donor hearts and by problems with tissue compatibility. Our work takes a step toward engineering tissue and whole organs specifically for each patient.”
It’s a big step, yet the path ahead is long. Asked when he expected that scientists would be able to build a whole human heart for implantation, 38-year-old Yang quipped, “Hopefully before I die.” That said, the results of this study may find significant application sooner—perhaps to regenerate heart-tissue patches for implantation or as a model to test cardiac drug therapies.
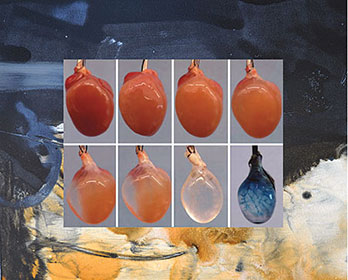
The group’s new approach starts with decellularized mouse hearts. And how do you get one of those? Researchers “wash out” the cellular content of a mouse heart using detergents and enzymes, removing virtually all of the cellular innards. What’s left is the so-called ECM, or extracellular matrix. ECM is basically the stuff that holds us together. It is secreted by fibroblasts, specialized cells that occur in connective tissue, and it retains its architecture after the cellular contents have been removed—providing a foundation upon which to build a new heart.
Researchers then seed what’s left of the mouse heart with human pluripotent stem cells, which have the potential to differentiate into organ-specific cells. The stem cells were coaxed into producing multipotential cardiac progenitor (MCP) cells. MCPs are precursors to three types of heart cells: cardiomyocytes, smooth muscle cells, and endothelial cells.
Once introduced to their new home and subjected to a complex diet of growth factors and other cellular delights, MCPs colonized the mouse heart scaffold and began to differentiate into the aforementioned three cell types. Even more significant: Specific cell types appeared right where they belonged. After 20 days of proliferation, the brand new heart construct started to beat spontaneously—though it was a little weak and slow by human heart standards.
Yang and his colleagues will next try to seed hearts so they produce a faster and more forceful beat. Success could send a lot of hearts racing.
